Update: 26 April 2024
Cost. What does hair analysis hTMA cost?
Contents
- What does it cost?
- Some hTMA Advantages
- Quitting Before Starting
- The Perception of Value
- Systemic Dysfunction - Medical and Insurance Industries
- Conclusion

The term wealth is derived from the Old English word weal which means well-being, literally.
What does it cost?
Many people save money with hTMA. The targeted nutrition information the test provides helps you avoid ‘nutritional roulette.’ You are able to focus your food and nutritional supplement spending, and purchase products that provide the greatest value. The overall improvements in health allows you save money on healthcare too.
Cost factors to consider.
- 1. First Cost Factor - Quality Food
- You must seek out and purchase non-toxic and nutritious food. This food is often more difficult to find and may cost more than cheap, subsidized, processed food (unless of course, you factor in the true environmental costs, human and animal rights cost, and healthcare costs). However, if you shop-smart by purchasing directly from the source, and purchase in bulk where possible, you might find that you do not spend any more than you are currently spending.
- 2. Second Cost Factor - Quality Time
- You have to prepare your food yourself. This takes time and knowledge. Also, it requires the proper equipment. For example, you will be purchasing non-toxic cookware, a high-quality low-speed masticating juicer, perhaps a food processor (not required) and a few other items. On the plus side, this will actually save you money because you will rarely be eating out at restaurants. Instead, you can get together with friends, cook and enjoy a good meal together. It's something we like to call, "fun!" And everyone benefits because you learn from each other.
- 3. Third Cost Factor - Money
-
Finally, there is the cost of the hTMA lab test. Similar to other medical tests that require a specialist's interpretation and analysis (e.g., radiological imaging), proper hTMA interpretation requires experience. Working with a qualified hTMA practitioner will typically cost $250 for an initial test, and $150 for a follow-up evaluation retest. Recommended supplements are extra (these will vary, depending on individual's specific needs).
Following your initial test, a progress retest is recommended (approximately every 2-6 months depending on the individual). The retest provides the data needed to evaluate the mineral pattern changes that occur. This data enables your practitioner to adjust your supplement profile so you can continue to improve.
- The Financial Bottom-line
- The bottom-line is that you may spend somewhere between $100 - 300 per month (depending on an individual's specific needs). However, supplement costs for children are generally a fraction of what a middle-aged person spends, and children respond to therapy much more quickly and easily. Unfortunately, because of the chronic nature of deterioration and the greater levels of dysfunction, more effort and time is required for most adults.
If hTMA sounds too expensive, consider the cost of poor health.
According to a Kaiser Family Foundation study "An estimated 1 in 3 Americans report having difficulty paying their medical bills. While the chances of falling into medical debt are greater for people who are uninsured, most people who experience difficulty paying medical bills have health insurance."
And when you compare using hTMA for preventive care with the true costs (i.e., not government subsidized) and incalculable personal costs of managing illness and disease with conventional medical treatment — hTMA is clearly the better choice.
Some Advantages of hTMA
hTMA is a medical test for diagnostic, screening and biomonitoring information. hTMA provides comprehensive information about health and performance status, and identifies trending toward disease.
- hTMA is more cost-effective than other biomonitoring tests (e.g., blood, urinalysis, radiological imaging).
- Hair is recommended by the EPA as the tissue of choice for the assessment of chronic toxic metal levels.
- Obtaining a hair sample is inexpensive, quick and easy, non-invasive and safe compared with a blood draw.
- Blood serum has self-protective homeostatic (balancing) mechanisms which affect trace element levels. This can present a misleading impression that everything is better than it may be.
- Chronic, long-term mineral changes (retention or losses) are more easily detected in hair than blood.
- Concentrations of most elements are significantly higher in hair than blood.
- Hair provides a biological activity record of past and present trace element levels.
Quitting Before Starting
Some people discard hTMA offhand because of "cost." But the financial cost is actually only one of several variables to consider for an accurate assessment of overall value. It makes good sense to understand and compare the value of hTMA verses its cost and not simply reject it based on cost alone. Not everything should be reduced to strict economic thinking.
Countless studies have shown that enjoying good health is the lowest-cost way to live a happy life.
So even from a financial perspective, cost is not a valid reason for postponing improving one's health. This fact is clearly illustrated with an objective comparison of the true financial cost of promoting and sustaining health, with the increasing costs associated with treating disease (and often supporting a long painful process of health deterioration). Health is an issue that goes much beyond mere financial cost. At its core, your health is really all about the quality and value of your life.
Physician training programs do not include hTMA (or corrective nutritional therapy) in their curriculum. Presently, a doctor's primary education is centered around surgical procedures and pharmaceuticals. And because hTMA is complex and not yet widely practiced, some people reject it without first adequately educating themselves. Most detractors are unqualified to comment either way because they have no training in hTMA, and are unaware of the supportive science and decades of successful clinical application. They may even feel threatened economically (i.e., if their business profits from the prevalent disease management paradigm), or they may feel their belief system is challenged (social, political, religious, or professional ideology).
The Perception of Value
Theoretically, ‘value’ refers to the perception of benefits received for what one must give up. So the financial cost of something reflects an important aspect of what one gives up in any transaction involving money. Therefore the (perceived) value will be affected by the (perceived) financial cost.
Truth and Misconception
The true cost of most transactions is not just financial. True cost often involves other things one may be giving up. For example, in addition to paying money, you may have to spend time educating yourself, and then you may need to change how you do some things.
The types of values promoted by the consumer-model lifestyle create a variety of problems for everyone. Scarcity is inherent in a system that encourages consumerism. With a consumer oriented system, corruption is inevitable because it is managed by the disproportional "one percent" at the top of the hierarchy (the few who actually benefit). There will never be enough money to acquire all that you desire, whether you are rich or poor. Until there is a paradigm shift in our values to those that are in sync with sustainability and humanity, we will feel distressed about money. Our ancestors understood that sustainability included values of cooperation, love, community, and respect for their health and their home planet.
There is a common misconception that the medicine provided by your doctor or hospital is safe because of oversight by the FDA.
The sworn purpose of the FDA is to protect the public health, to assure us that all the drugs on the market are proven safe and effective by reputable scientific trials. Yet, over and over again, the agency has proven itself willing to keep scientists, doctors, and the public in the dark about incidents when those scientific trials turn out to be less than reputable. It does so not only by passive silence, but by active deception. It actively buries evidence of fraud in medical trials.
When the FDA finds scientific fraud or misconduct, the agency doesn't notify the public, the medical establishment, or even the scientific community that the results of a medical experiment are not to be trusted. On the contrary. For more than a decade, the FDA has shown a pattern of burying the details of misconduct. As a result, nobody ever finds out which data is bogus, which experiments are tainted, and which drugs might be on the market under false pretenses.
The FDA buries evidence of fraud in medical trials.
Systemic Dysfunction - Problems with the Medical and Health Insurance Industries
It is health that is real wealth
and not pieces of gold and silver. Mahatma Gandhi
Despite the for-profit health insurance industry's rhetoric, the best health insurance is actual health. And when an industry is powerful enough to get laws enacted which force people to purchase their products, shouldn't their motives and actions be carefully and objectively assessed?
The average health insurance premium for an individual in the US is $235.27 per month. The average family premium per enrolled employee for employer-based health insurance is $15,473. It is getting harder for an average family to pay this much for something with so little real value. This enrichment of the health insurance industry is literally forcing families to compromise their own health, because after paying their premium and co-pay fees they cannot even afford to buy good food. Does this make any sense to you?
The high-cost of poor health is becoming too much of a burden to pay. Maintaining one's own good health is a bargain compared to the physical suffering and financial misery associated with conventional symptom suppression therapies (i. e., invasive tests, toxic drugs, dangerous surgeries, etc.). Health insurance actually masks the true costs of conventional "healthcare." Making use of the conventional medical system's technologies and drugs is in fact, very expensive. It is so expensive that all of the political and medical industry debate revolves around cost reduction. The insurance industry imposes increasingly restrictive time limitations on the doctor-patient relationship, and promotes faster, cheaper therapies. Therapy which often times focuses on short-term symptom suppression rather than restoring actual health. When cost-cutting policies override clinical expertise and the quest for healthcare excellence, the very real healthcare needs of the individual pays a terrible price. In the new "managed care" paradigm, freedom of healthcare choice is the first casualty. Such an approach to healthcare is inherently unhealthy.
- The voices of patient harm More than 1 million patients suffer harm each year in U.S. health care facilities. Often, their harm isn't acknowledged even as they live with the consequences — ProPublica
Institute of Medicine (IOM) Report: Best Care at Lower Cost
The following excerpt is from the preface of an exhaustive 381 page report which highlights fundamental problems within the dysfunctional American health care system.
The tragic life of Dr. Ignaz Semmelweis offers an example of the challenges faced in building a truly learning health care system. In 1847, the Hungarian physician observed that simply washing hands could drastically reduce high rates of maternal death during childbirth. Semmelweis's observations conflicted with the established scientific and medical opinions of the time and his ideas were rejected by the medical community. Since he could not prove a connection between hand washing and the spread of infection, he was ridiculed and ignored.
In 1865, Semmelweis was committed to an asylum, where he died at age 47 after being beaten by the guards, only 14 days after he was committed. More than 165 years later, half of clinicians still do not regularly wash their hands before seeing patients. The challenges today are in some ways that straightforward, and in many other ways significantly more complex. Narrow-minded rejection of scientific evidence is rarely encountered today in medicine, yet the American health care system imposes significant institutional, economic, and pedagogic barriers to learning and adapting.
For more than a decade, reports of the Institute of Medicine (IOM) have focused attention on a persistent set of problems within the American health care system that urgently need to be addressed, including:
- poor quality
- high cost
- questionable value
- mal distribution of care based on income, race, and ethnicity.
Each report has called for substantive transformation of the nation's health care system. Many have pointed out a disturbing paradox: the coexistence of over treatment and under treatment. The committee that authored this report found a similar situation: learning and adoption that are maddeningly slow — as with hand washing — coexisting with overly rapid adoption of some new techniques, devices, and drugs, with harmful results.
Source: https://www.nap.edu/. Published by the National Academies Press (NAP) was created by the National Academy of Sciences to publish the reports of the National Academy of Sciences, National Academy of Engineering, Institute of Medicine, and National Research Council, all operating under a charter granted by the Congress of the United States.
Inconsistent and Grossly Unfair Billing by Hospitals
Excerpt form a Huffington Post exposé: Americans have long become accustomed to bewilderment and anxiety when confronting health care bills. The new database underscores why, revealing the perplexing assortment of prices for medical care, with the details of bills seemingly untethered to any graspable principle. Even within the same metropolitan area, hospitals charge prices that differ by staggering degrees for the same procedures. People without health insurance pay vastly higher costs for care when less expensive options are often available nearby. Virtually everyone who seeks health care winds up paying inflated prices in one form or another as these stark disparities in price sow inefficiencies throughout the market. Read the full article
There are many parts of the health care delivery and financing systems that urgently need updating, and the matter of ‘charges’ is among those at the top of the list. The complex and bewildering interplay among ‘charges,’ ‘rates,’ ‘bills’ and ‘payments’ across dozens of payers, public and private, does not serve any stakeholder well, including hospitals. Rich Umbdenstock, president and CEO of the American Hospital Association
The cost of healthcare is out-of-control. The United States healthcare tab for 2009 was $2.5 trillion, representing 17.3 percent of the nation's gross domestic product (profits that depend on people's failing health). The Health and Human Services Department expects that the health share of GDP will continue its historical upward trend, reaching 19.5% of GDP by 2017. This is an unsustainable rate of growth. Thirty-two percent of Americans put off medical care for themselves or their family due to the cost. Medical bills are the cause of more than 60 percent of all bankruptcy filings.
Physician Burnout and Depression is a Serious Concern (can lead to major medical errors)
SOURCE: abcnews.go.com/Health/physician-burnout-depression-lead-major-medical-errors-study
A recent study found, 55 percent of doctors reported symptoms of burnout, 33 percent had high levels of fatigue, and 6.5 percent had thoughts of killing themselves in the last year. According to the study, doctors have 3 to 5 times the suicide rate of the general public.
Medical errors are more than twice as likely if a doctor has signs of burnout, and 38 percent more likely if they have signs of fatigue. Just over 10 percent of doctors reported making a major medical error in the three months before the survey, with about 1 in 20 of these errors being fatal. The most common mistakes were "errors in judgment," followed by incorrect diagnosis and technical errors.
What's also concerning, an article an international peer reviewed medical journal, The BMJ (formerly the British Medical Journal) reports conventional medicine is the 3rd leading cause of death in the U.S. And there is more recent compelling evidence which suggests it is #the 1 cause.
U.S. Health in International Perspective: Shorter Lives, Poorer Health (report excerpt)
Important antecedents of good health are also frequently problematic in the United States. What should the nation should do about the U.S. health disadvantage? We believe that there is sufficient evidence for the country to act now, without waiting for additional research. The pervasiveness of the U.S. health disadvantage and the fact that it has been worsening for decades leads us to recommend that the nation and its leaders act now in three areas:
- Intensify efforts to pursue existing national health objectives that already target the specific areas in which the United States is lagging behind other high-income countries.
- Alert the public about the problem and stimulate a national discussion about inherent trade-offs in a range of actions to begin to match the achievements of other high-income nations.
- Undertake analyses of policy options by studying the policies used by other high-income countries with better health outcomes and their adaptability to the United States.
Download: U.S. Health in International Perspective: Shorter Lives, Poorer Health
Drowning in Medical Debt
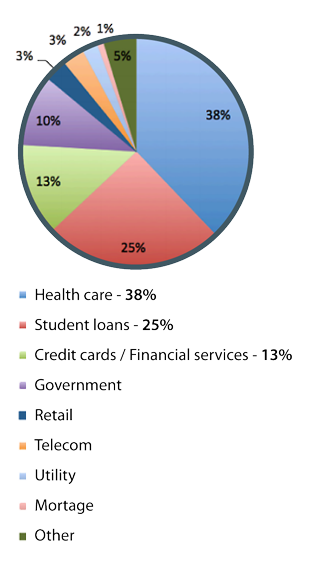
In America, healthcare is the number-one cause of personal bankruptcy and is responsible for more collections than credit cards. Americans pay three times more for medical debt than they do for bank and credit-card debt combined, the report found. Nearly a fifth of us will hear from medical-debt collectors this year, and they'll gather $21 billion from us, collectively.
Roughly 40 percent of Americans owe collectors money for times they were sick. U.S. adults are likelier than those in other developed countries to struggle to pay their medical bills or to forgo care because of cost.
Another contributing factor is that hospitals charge wildly different amounts for the same procedures. Patients have few options beyond attempting to research hospital charges ahead of time—which is probably the furthest thing from a person's mind when they are most in need of a hospital.
Excerpt from a Wall Street Journal article
Our ‘health-care system’ is primarily a disease-care system. Last year, $2.1 trillion was spent in the U.S. on medical care, or 16.5% of the gross national product. Of these trillions, 95 cents of every dollar was spent to treat disease after it had already occurred. At least 75% of these costs were spent on treating chronic diseases, such as heart disease and diabetes, that are preventable or even reversible.
(Heart disease) The disease that accounts for more premature deaths and costs Americans more than any other illness is almost completely preventable simply by changing diet and lifestyle. The same lifestyle changes that can prevent or even reverse heart disease also help prevent or reverse many other chronic diseases as well.
When you eat a healthier diet, quit smoking, exercise, and have more love in your life, then your brain receives more blood and oxygen, so you think more clearly, have more energy, need less sleep. Your brain may grow so many new neurons that it could get measurably bigger in only a few months. Your face gets more blood flow, so your skin glows more and wrinkles less. Your heart gets more blood flow, so you have more stamina and can even begin to reverse heart disease. Your sexual organs receive more blood flow, so you may become more potent — similar to the way that circulation-increasing drugs like Viagra work. For many people, these are choices worth making — not just to live longer, but also to live better.
Conclusion: hTMA - Affordable healthcare, and the best health insurance.
The health insurance industry supports a medical system model that does not profit from health. Conventional medical services play an important role, especially in life-saving emergency care. But. The medical industry profit model relies on surgical procedures, pharmaceutical drugs, etc. You will not receive financial support from insurance companies to help you build and maintain good health. So, caring for your health is something that you must pay for with your own time and money. With the current medicine-for-profit paradigm, the inevitable cost of poor health is financial ruin. Alternatively, hTMA is proven effective, is affordable and it enables you to attain your highest potential level of health.
If you value your health, the cost of hTMA is easy to justify. Even if all you care about is money — hTMA makes good sense.
Back to Top Find a hTMA Practitioner